Cannabis legalization associated with temporary reduction in opioid-related emergency room visits
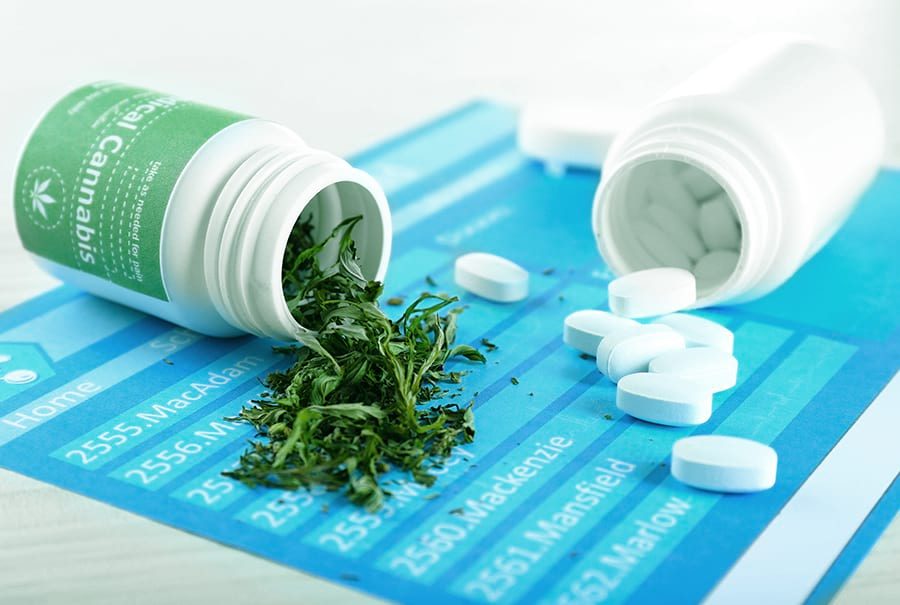
Could the opioid epidemic be curbed with cannabis? According to a team of scientists at the University of Pittsburgh Graduate School of Public Health, the rate of opioid-related visits to hospital emergency rooms in each cannabis-friendly U.S. state sank for approximately six months post-legalization.
In particular, the trend was most noticeable among all adults aged 25-44 years old, as well as the male demographic. Typically, opioid-related emergency department visits reduced by 7.6 percent in the six months after adult-use cannabis laws were implemented.
Information was gathered from the Healthcare Cost and Utilization Project (HCUP) Fast Stats database for this investigation into the effect(s) of cannabis legalization on opioid-related emergency visits.
Included in the analysis was data pertaining to the number of opioid-associated hospital visits per 100,000 population; as reported by each cannabis-friendly state in quarterly intervals.
Inpatient admissions were recorded for each visit, in addition to treat-and-release visits for every type of opioid-related visit, such as withdrawal symptoms, opioid-triggered psychosis and opioid toxicity/poisoning.
Researchers merged data with information on state-level recreational and medical cannabis legalization implementation dates, in addition to various other kinds of opioid-related state policies.
This information was gleaned from socioeconomic characteristics data featured in the American Communities Survey, as well as the RAND-USC Schaeffer Opioid Policy Tools and Information Center.
An overview of the opioid crisis in the U.S.
Since 2017, the United States Department of Health and Human Services has declared the nation’s opioid crisis a public health emergency. The year prior to the health crisis’ confirmation, 42,000 fatal drug overdoses were recorded in the U.S., where in excess of 81,000 drug overdose deaths occurred from June 2019 to May 2020.
According to the Centers for Disease Control and Prevention (CDC), these figures represent the highest number of overdose deaths ever to be recorded in a 12-month timespan. In most cases, drug overdoses are triggered by the rising use of synthetic opioids like fentanyl. Moreover, drug-related mortalities in the U.S. are stimulated by illicit drug use, with heroin and/or fentanyl-contaminated cocaine being a primary cause of death.
These worrying figures accentuate the need to address problems with opioid abuse and addiction. With a new study published in Health Economics showing that states with legal recreational cannabis seem to record fewer opioid-related emergency department visits, it’s possible that the plant could harbor potential to save tens of thousands of lives every single year.
Data was pulled from 29 states for study on cannabis and opioid-related emergency visits
In total, data was analyzed from 29 different states for this investigation into the effect of cannabis legalization on opioid-related emergency room visits. The quarterly information, which was logged between the years 2011 and 2017, was sourced from the Fast Stats database.
During this time period, California, Maine, Massachusetts and Nevada – all of which were included in the dataset – passed recreational cannabis laws. The remaining 25 states were simply used as controls. Four other states, Alaska, Colorado, Oregon, and Washington, were excluded from the analysis.
Researchers noted that the dip was mainly spurred on by shrinking admission rates from the male demographic. Moreover, admissions reduced – albeit to a slightly smaller extent – among adults aged 25-44 years old.
After approximately two quarters, the distinguishable reduction in emergency room visits returned to baseline levels; it’s important to note that these visits did not surpass the baseline.
“This isn’t trivial—a decline in opioid-related emergency department visits, even if only for six months, is a welcome public health development. But that being said, while cannabis liberalization may offer some help in curbing the opioid epidemic, it’s likely not a panacea,” said the study’s lead author Coleman Drake, Ph.D.. He also assumes the role of assistant professor in the University of Pittsburgh’s Department of Health Policy and Management.
Drake noted that the team could not definitively conclude why recreational cannabis laws are linked to a temporary downturn in opioid-related emergency department visits. However, he emphasized that the findings, combined with previous literature, suggest that opioid users are turning to cannabis as a substitute.
“Cannabis can provide pain relief for persons using opioids, but cannabis ultimately is not a treatment for opioid use disorder. Still, this is good news for state policymakers. States can fight the opioid epidemic by expanding access to opioid use disorder treatment and by decreasing opioid use with recreational cannabis laws. These policies aren’t mutually exclusive; rather, they’re both a step in the right direction,” Drake concluded.