CNB Exclusive Interview: Lead doctor in study explains patients’ switch from prescriptions to cannabis
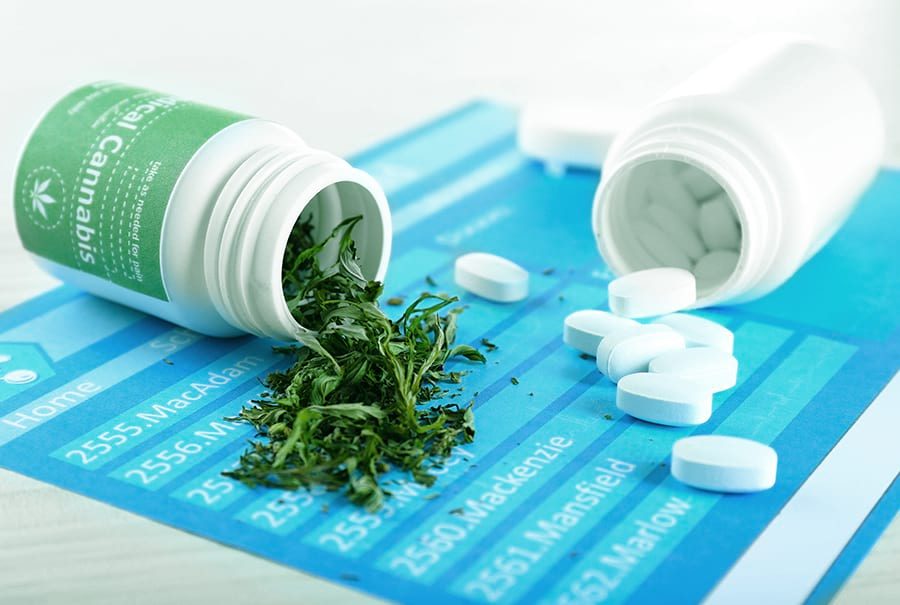
In a soon-to-be-published study from the Journal of Medical Directors Association, University of New Mexico researchers found medical cannabis patients reduced their intake of prescription drugs after months of enrollment in the Medical Cannabis Program.
Reports utilized the New Mexico Prescription Monitoring Program which listed all patient prescription records for the study. Seventy-one percent of medical cannabis patients either stopped or reduced their use of prescriptions within six months of enrolling into the state’s Medical Cannabis Program. Patients enrolled lowered their monthly average number of prescriptions, number of prescribers, types of prescriptions, and related pharmacy visits.
Cannabis News Box sat down with Dr. Anthony Reeve, the study’s treating clinician, to discuss the findings and receive additional information about medical cannabis reducing prescription medications.
CNB: What inspired the researchers from the University of New Mexico and the Industrial Rehabilitations Clinics of Albuquerque to conduct this study? Did the high level of opiate prescriptions in New Mexico influence the decision to perform the study? If so, in what ways?
The primary inspiration for performing this type of research was in the initial phase of implementation of the Medical Cannabis Program. The majority of patients that I saw anecdotally reported to me that they were reducing their use of opiates and other prescriptive medications. The high use of opiates in New Mexico is well-known, [and] we were able to implement this research program to evaluate the studies of medical cannabis on the reduction of opiates and other scheduled medications. The timing of the study is more appropriate to current events than it was 3 years ago [before the crisis was acknowledged].
CNB: While most studies on medical cannabis view state-level outcomes, why do you think your study is the first to examine individual patients on a direct level when there are other states where cannabis is legal?
This study is important because it actually followed [groups] of patients after the implementation of the Medical Cannabis Program. Other studies [were looked at] such as the Ohio study which documented decreased opiate use after its medical cannabis program was instituted. There was an additional study which looked at Medicare costs associated with prescriptions [and showed a decreases in prescription costs] when measured after medical cannabis legislation was passed. Ours is the first study that looks at an individual patients and measures them against a pharmacy monitoring program. The study included a control group which either increased their use of prescriptions or remained the same. This allows for the individual argument of specific patient results rather than large observational studies.
CNB: Were there any surprise breakthroughs your team made during research which was not widely known before?
[We were surprised to find] there was a reduction of all medication classes, including opiates. This included drugs placed Schedule II through V, as well as the number of prescriber’s cost.
CNB: Do you think conducting this research in another medical cannabis program would have provided different results?
I do not believe different results would occur if the protocol followed for a larger population. I believe the study is strong and would be reproducible with an even larger group of patients.
CNB: Were there any factors for choosing New Mexico as your preferred medical cannabis market to research?
At the time, the requirements of having a pain doctor as a certifying physician made it possible to gather a large group of patients for study. In addition, New Mexico was in the early stages of the physician monitoring program, which meant the study could be utilize the monitoring program in documenting the actual findings and reduction of prescription medications. The prescription monitoring program is an independent governmental agency which is not subject to bias or consideration.
CNB: 71 percent of medical cannabis program enrollees either ceased or reduced their use of scheduled prescriptions within 6 months of enrolling; What could be said for the 29 percent which did not reduce their prescriptions after enrolling in the medical cannabis program?
Not much can be said about the 29 percent which did not reduce her prescriptions after enrolling in the Medical Cannabis Program. The 29 percent gives legitimacy to the study. It is not reasonable to expect 99 percent of all cannabis users would reduce prescription use. Cannabis is not a cure-all for every symptom, and with all patients, it can be stated to a reasonable degree of medical probability that intervention had a significant effect on decreased use. If we had not found the 29 percent it would have imposed significant doubt into the study’s findings.
CNB: Aside from opiates, benzodiazepines and sleeping medications, were there other specific medications which researchers saw a drop in use after enrolling in the medical cannabis program?
It was found that all medications Schedule II through V had reduction in utilization. This category encompasses all medications [which require a prescription].
“The question at this point is whether medical cannabis is a gateway drug. Does that gateway swing both ways? Could medical cannabis be utilized as a step down from the use of opiates, or a transitional medicine to get patient’s off of opiates altogether?”
CNB: Do the results of this study have the potential to help other researchers in addressing the opioid epidemic nationally? In what way?
Yes, the study has potential for researchers to address the opioid epidemic nationally. The question at this point is whether medical cannabis is a gateway drug. Does that gateway swing both ways? Could medical cannabis be utilized as a step down from the use of opiates, or a transitional medicine to get patient’s off of opiates altogether? Clinical research does show cannabis does affect pain appreciation, but the question remains: Can cannabis be used as a substitute for chronic pain? This is a more difficult question because chronic pain is by far the leading cost driver and the significant utilizer of opiates.
CNB: Health Secretary Lynn Gallagher recently denied adding opiate use disorder to the state’s list of qualifying conditions, and there has also been push by the legislature to add opiate use disorder to the program. Given the results of this study, do you have any thoughts as to if it should be added as a qualifying condition?
In my opinion, it would only be redundant to have opiate use disorder as a qualifying disorder, since chronic pain is already included as one of the qualifying conditions. Almost all patients who have chronic pain are on opiates and [adding the condition] would only be redundant.
CNB: What were the conditions the study participants used medical cannabis for? Did their conditions have any correlation with their opiate use?
The primary diagnosis associated with this study was failed back pain syndrome, or patients who had surgical intervention but continue to suffer from chronic back pain. This diagnosis was divided into lower back and cervical spine issues, which were the most common conditions. Other diagnoses included arthralgia and rheumatoid arthritis, [with some joint pain] after surgical intervention.
CNB: What doors do you think this study will open for future research?
In my opinion future research will focus on administration of the cannabis and dosing specific requirements. Future research needs to demonstrate the medicinal uses of cannabis [in relation to] appropriate dosage, timing, and appropriate follow-up for utilization. Long-term studies utilizing cannabis are virtually unknown and we do not know what the consequences of chronic use can mean for patients.
CNB: Do you have any relationship with medical cannabis, outside of a research capacity?
I am a partner at SBS Laboratories, a licensed provider of laboratory services to the cannabis industry in New Mexico, which evaluates potency and microbiology.
CNB: Thank you for sitting down with us today. Do you have any additional comments?
The issue of potency of the [medical cannabis] and the growers trend towards either changing the natural state of the cannabis plant, or increasing THC levels and CBD levels through concentration and extraction techniques. Almost all studies conducted on dosing and utilization were written in the 1960s and 1970s, and used the natural plant [which contain] THC levels of between 12 to 16 percent and lower CBD levels. Utilization of higher doses of THC and CBD may have unknown or even dangerous effects that we are unaware of. This could be the undoing of this industry and its infancy by allowing experimentation to be conducted on a live patient population.